
A 29-Year-Old Woman Saw Doctors About a Mole, but They Dismissed It – Later She Learned She Had Aggressive Skin Cancer
When a London woman noticed a dark spot on her scalp, a specialist dismissed the possibility of melanoma. Another diagnosed it as a fungal infection. By the time someone took her concerns seriously, the life-threatening disease had already spread to her skull.
Sarah Lee knew her body. So when a dark mole suddenly appeared on her scalp, she didn't ignore it. She went to the doctor. But instead of answers, she was dismissed. Not once, but three times.
What unfolded next was a startling reminder of how easily warning signs can be overlooked and how deeply trust in medical judgment can falter. At just 29, Sarah was about to discover the harsh reality behind her instincts and the silent threat hiding in plain sight.
Lee's concern deepened with each passing week, and she returned to her general practitioner to report the changes.
It was the summer of 2021 when Lee took a photo of her scalp, not out of concern, but to check if she needed highlights. Pandemic disruptions had made salon visits rare, and she wanted to see how much her hair had grown out.
In the photo, she spotted something unfamiliar: a pea-sized, black mole nestled in her fine blonde hair. She was sure it hadn't been there before. The next day, she called her general practitioner.
Lee was then referred to a dermatologist who examined the mole using a dermatoscope, a handheld device used to inspect skin lesions.
After the assessment, Lee was told three things: that the mole didn't look suspicious, that she was too young for skin cancer, and that it was nearly impossible to develop melanoma on the scalp because the hair protects from ultraviolet radiation. None of those statements was accurate.
Over the next five months, the mole began to change. It grew in size, darkened, and multiplied. Lee's concern deepened with each passing week, and she returned to her general practitioner to report the changes. This time, the lesion was visibly different.
It was blue-black and spreading. Still, her concerns were dismissed. The doctor told her the growth was a fungal infection and would go away on its own. No further action was taken.
Lee knew something wasn't right. She had already been told the mole was harmless, but what she was seeing and feeling told her otherwise.
Frustrated and unsettled, Lee decided to push for a second opinion. She arranged to see a different doctor in December 2021. This time, her concerns were met with urgency. The new dermatologist examined the spots on her scalp and responded immediately:
"I'm glad you came. I'm really concerned about these spots on your head."
Without delay, the moles were removed and sent for biopsy. After the procedure, Lee had a sizeable scar across her scalp, but no clear answers yet. As the holidays approached, she entered a stretch of waiting that was marked by rising anxiety.
In early January 2022, Lee received a call from a nurse with the results of her biopsy. The diagnosis was stage three malignant nodular melanoma, and it had already reached her skull. The news left her stunned and she nearly collapsed after the call.
Lee didn't use tanning beds, she always wore SPF 30 sunscreen, and she had grown up in Wales, where, as she put it, "it almost always rains." The diagnosis raised questions such as: How much time did she have left? Would she lose her hair? Why had three separate doctors told her she had nothing to worry about?
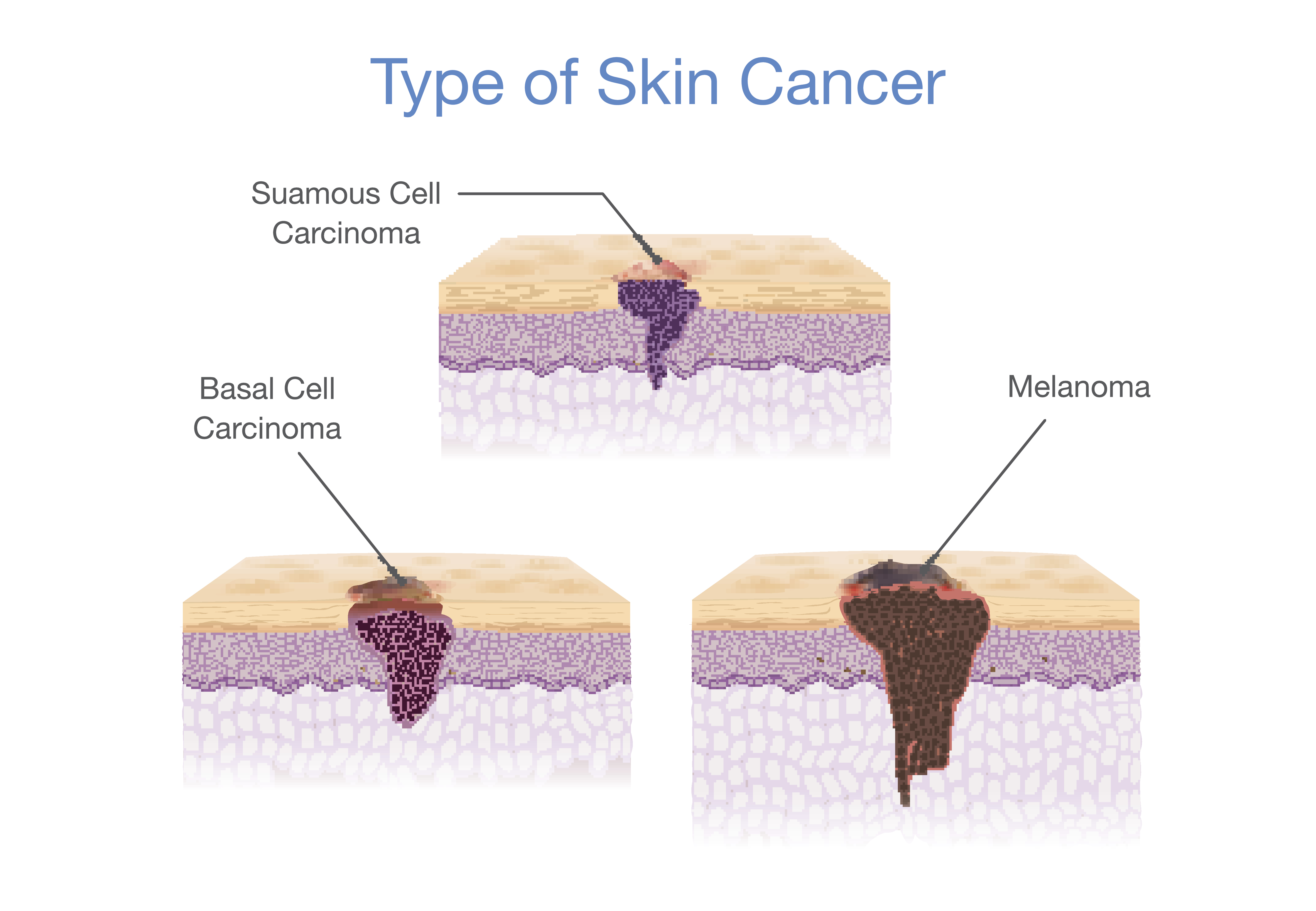
Melanoma is the most invasive type of skin cancer and carries the highest risk of death. It accounts for only about 1 percent of all skin cancer diagnoses but causes the majority of skin cancer-related fatalities.
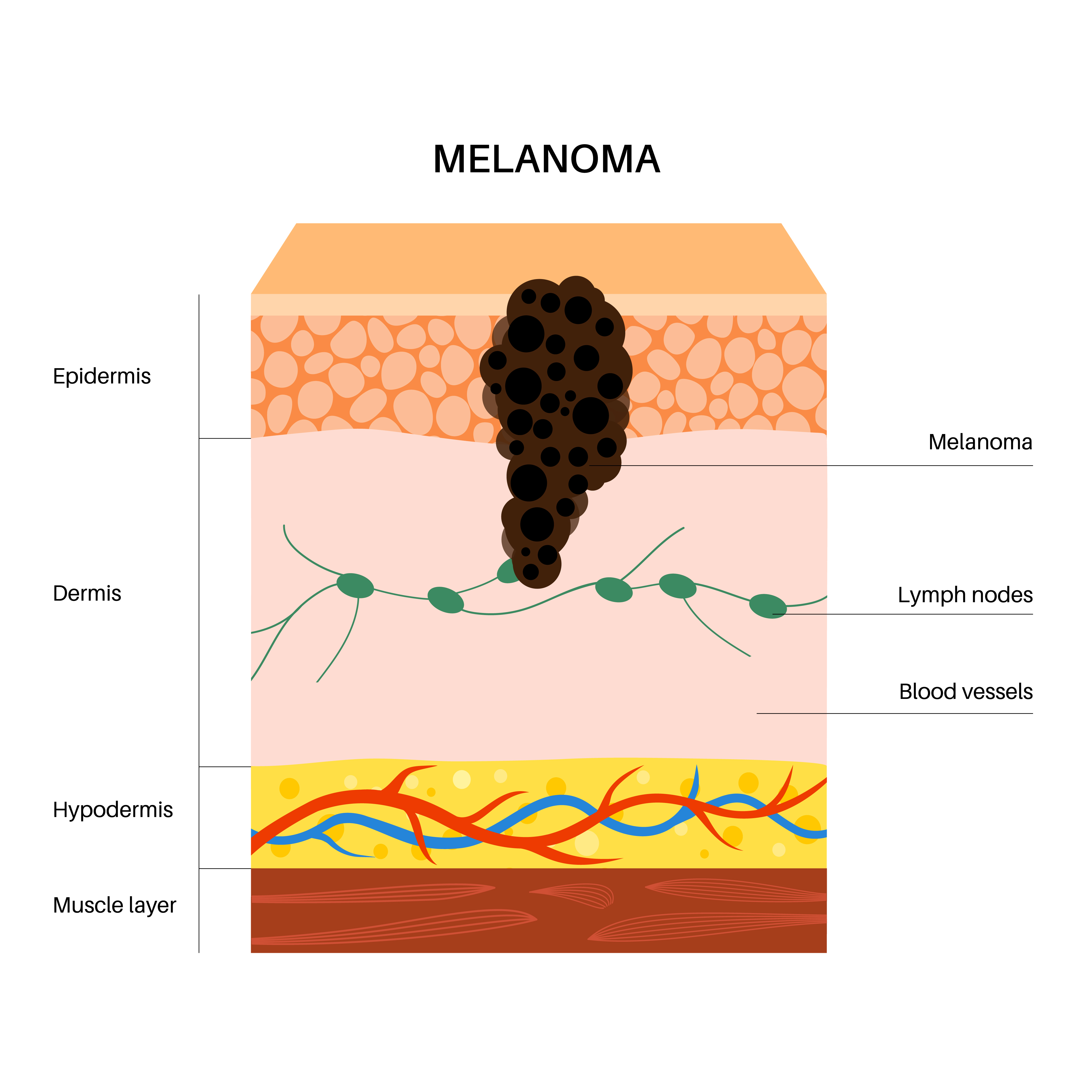
In Lee's case, the diagnosis was stage three malignant nodular melanoma, known for growing deeper into the skin more rapidly than other types. This type of cancer begins in the melanocytes, the cells responsible for skin pigment, and is known to spread rapidly into surrounding tissue, lymph nodes, and organs.

Young woman with a birthmark on her neck, highlighting concerns raised on World Melanoma Day about the importance of monitoring skin changes for signs of cancer | Source: Getty Images
Early detection significantly increases the chances of survival, but the disease becomes more difficult to treat once it spreads beneath the surface. However, melanoma can be difficult to detect, especially when it appears in places like the scalp.
Many cases begin as moles or dark patches that change over time. A major risk factor for melanoma is ultraviolet radiation, also known as UV radiation. These are invisible rays that come from the sun and artificial sources, such as sun lamps and tanning beds.
Types of skin cancer illustrated in 3D vector style Medical depiction | Source: Getty Images
Two types of UV rays reach the Earth's surface: UVA and UVB. Both can damage skin cells, accelerate aging, and increase the risk of melanoma and other skin cancers. UV exposure can also harm the immune system and the eyes.
Medical experts recommend broad-spectrum sunscreen, which protects against both UVA and UVB rays. UV radiation is also used in controlled medical settings to treat conditions such as psoriasis, vitiligo, and skin-related lymphomas. However, outside of those settings, unprotected exposure poses serious health risks.

Close-up of a woman's shoulder mole being marked for treatment by a doctor | Source: Getty Images.
Although Lee didn't use tanning beds and consistently wore SPF 30, she had several risk factors: fair skin, light hair, and a mole that appeared in a difficult-to-monitor area. Melanoma often starts as a new or changing mole, and dermatologists advise using the "ABCDE" system to help identify warning signs:
- Asymmetry — one half of the mole doesn't match the other
- Border — edges are ragged or uneven
- Color — multiple or uneven shades
- Diameter — larger than 6 millimeters
- Evolving — any change in size, shape, or color
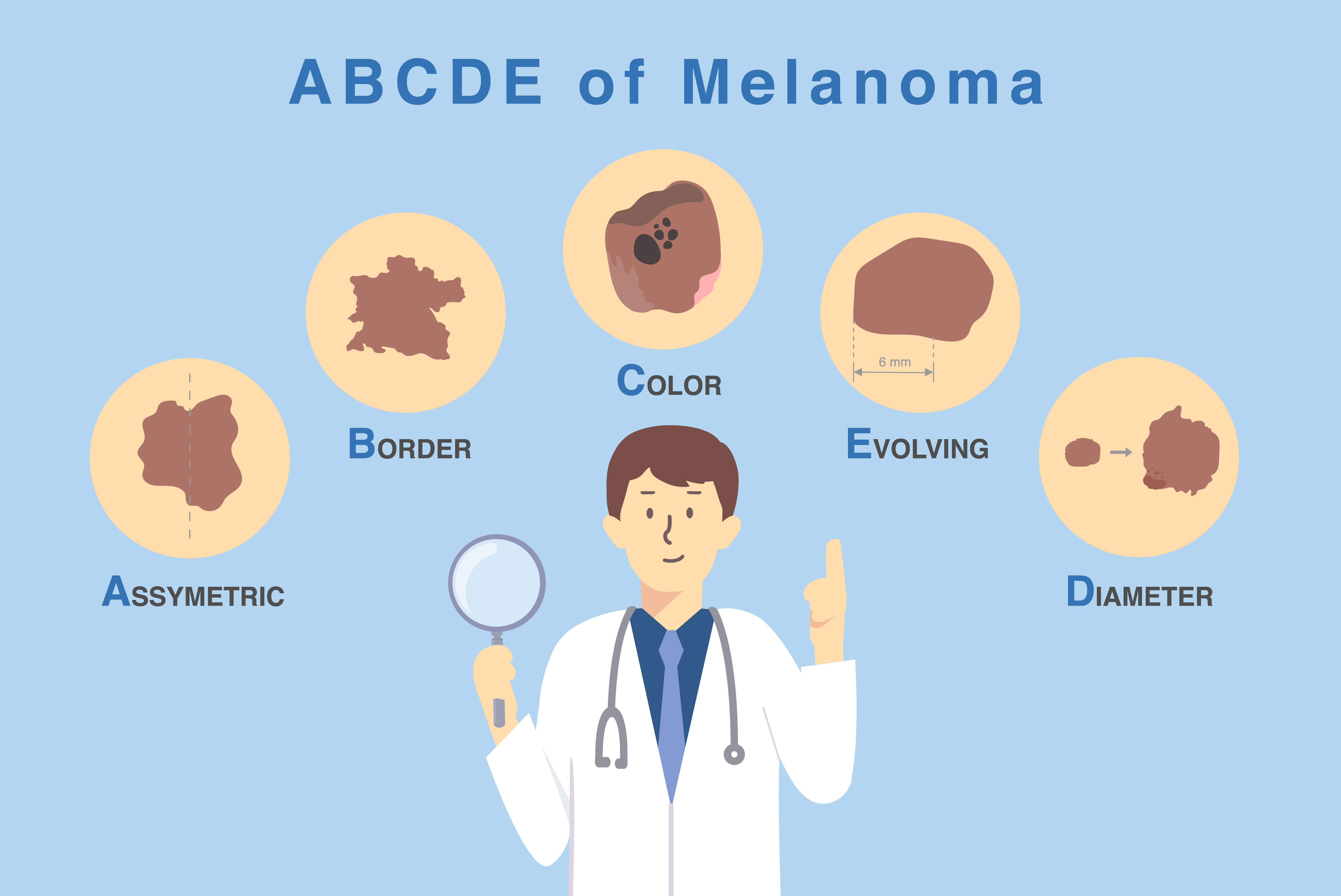
Doctor holding a magnifying glass over five key characteristics of skin damage, demonstrating the ABCDE method for diagnosing and classifying melanoma | Source: Getty Images
Some melanomas don't fit these criteria. A separate guideline known as the "ugly duckling" sign urges people to look for any spot that stands out from the rest. With the diagnosis confirmed, she was sent for a series of scans — CT, MRI, and PET — to find out whether the cancer had spread beyond the skin and bone.
Lee experienced nausea, vomiting, fever, fatigue, and rashes, sometimes all at once.
The scans revealed that the cancer had already reached a lymph node on the left side of Lee's neck. Treatment would require a radical dissection, an extensive surgical procedure to remove all of the lymph nodes and surrounding tissue in the affected area.
3D vector illustration of different types of skin cancer – medical visualization | Source: Getty Images
The word "dissection" stuck with her, bringing back a memory from school when she had to cut into a sad-looking fish during a Year 11 biology class. Now, she would be the one on the table. The operation was scheduled for March 11, 2022, at the Royal Free Hospital in Hampstead and would take eight hours.
When it was over, Lee was sent home with a surgical drain to collect blood and fluid from the site. She carried it with her for two weeks as she began a slow and painful recovery. Follow-up scans showed no visible signs of remaining cancer. However, treatment wasn't over.

Sarah Lee, seen in a post dated January 15, 2022 | Source: X/sarahkatelee
To reduce the risk of recurrence, Lee began a 12-month course of targeted therapy: dabrafenib and trametinib. The drugs are designed to block cancer growth at the molecular level and are commonly used in advanced melanoma cases with specific mutations.
The side effects were immediate and severe. Lee experienced nausea, vomiting, fever, fatigue, and rashes, sometimes all at once. The regimen was grueling but necessary. Taking the medication gave her a 75 percent chance of keeping the cancer from returning.
Her life adjusted to a new rhythm of medications, blood tests, and constant monitoring. The physical symptoms were only part of it. The mental weight of the diagnosis and everything that had led to it had not lifted.
The psychological aftermath set in quietly but firmly. From someone who had once enjoyed the sun, Lee now avoided it completely. From someone who trusted medical advice without hesitation, she had grown fearful of accepting any diagnosis at face value.
The illness had changed more than her body. It had altered how she moved through the world. She later wrote:
"I am terrified of the cancer coming back. And I'm angry it could have been spotted sooner."
Even as her body healed, anxiety lingered over every scan, every check-up, every new mark on her skin. The threat no longer felt theoretical. It had already happened once. As Lee continued treatment, she began sharing her experience publicly.
In interviews and personal writing, she emphasized that melanoma is often misunderstood. "People see skin cancer as the nicer or lesser cancer," she said. "But when it gets to your organs, it can spread like wildfire. It can hide and lay dormant and come back years later."
She also pushed back against the idea that a tan signals health. "Any kind of tan is unhealthy," she commented. "Any changes in the color of your skin due to the sun is skin damage which increases your risk of skin cancer. Left untreated, this can spread to your vital organs and be a lot harder to treat. It's really not worth it."
Lee also turned to social media to reach others who might be at risk. On January 15, 2022, just days after receiving her diagnosis, she posted, "Please check your moles, trust your gut, and get a second/third/fourth opinion."
Her posts drew attention to something she now repeats often: early detection can be life-saving, and persistence can make the difference between a delayed diagnosis and timely treatment. Her message is especially urgent for anyone with fair skin or hard-to-see areas like the scalp, where melanoma can develop unnoticed.
On May 4, 2023, Lee marked a major milestone: the final day of her melanoma treatment. She shared the update online, writing, "Today marks the end of my melanoma treatment (finally!) It's been a long time coming."
She also cautioned her fans and followers, noting, "Whilst I hope the disease is behind me, my message is the same—look after your skin. It's your biggest organ!!"
The treatment may have ended, but her commitment to skin cancer awareness didn't. For Lee, the experience left permanent scars, some visible, some not, but also a determination to make sure others don't ignore the signs she was once told not to worry about.
The information in this article is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, and images contained on news.AmoMama.com, or available through news.AmoMama.com is for general information purposes only. news.AmoMama.com does not take responsibility for any action taken as a result of reading this article. Before undertaking any course of treatment please consult with your healthcare provider.
